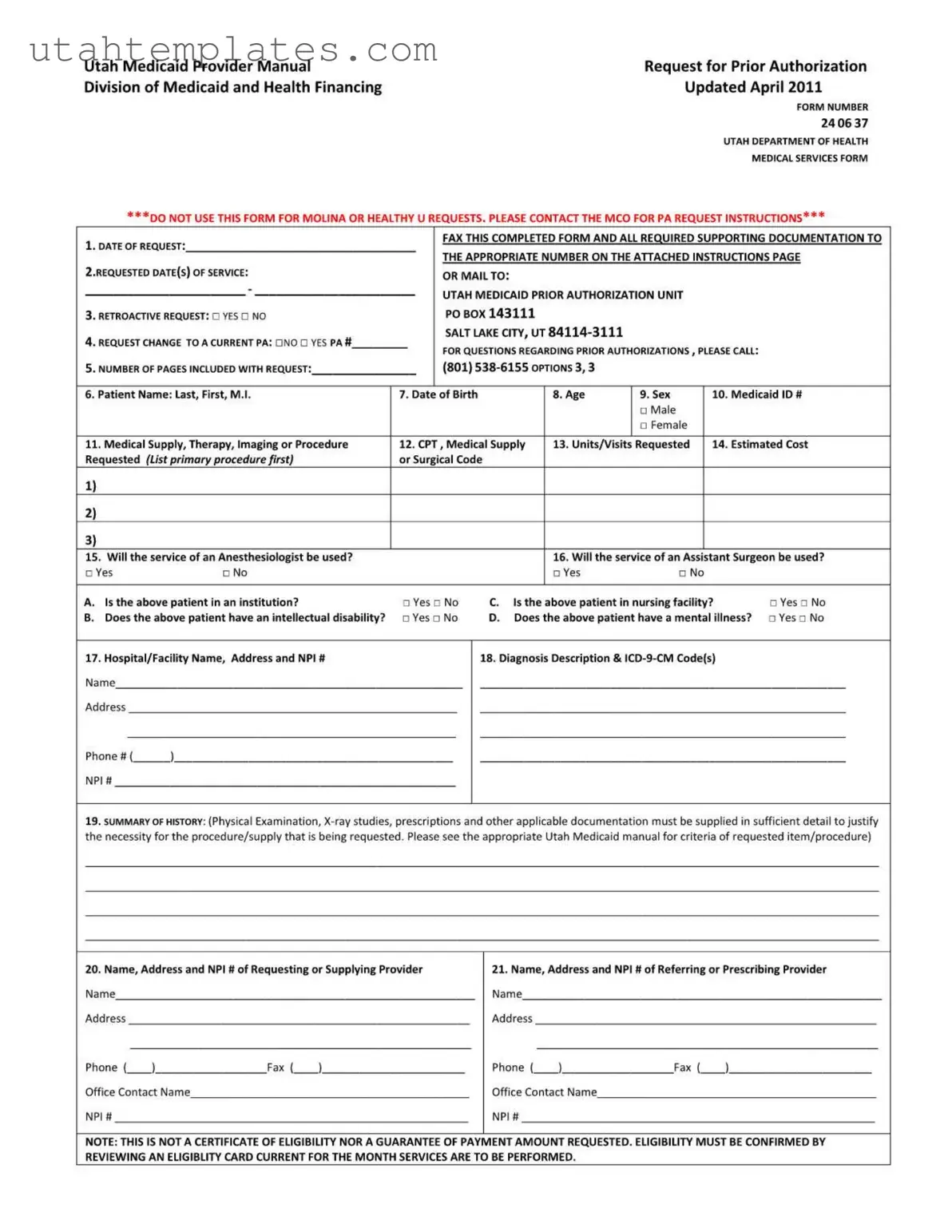
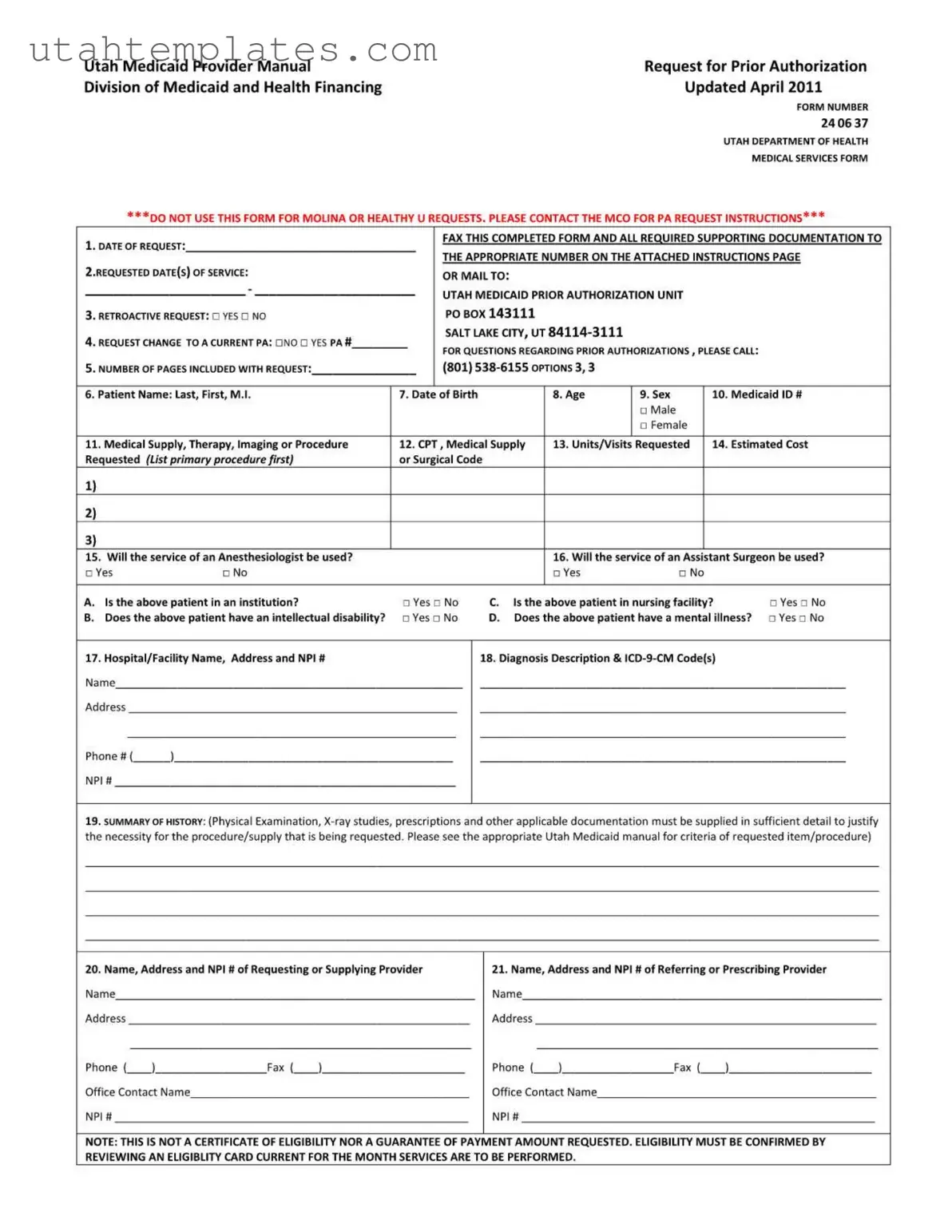
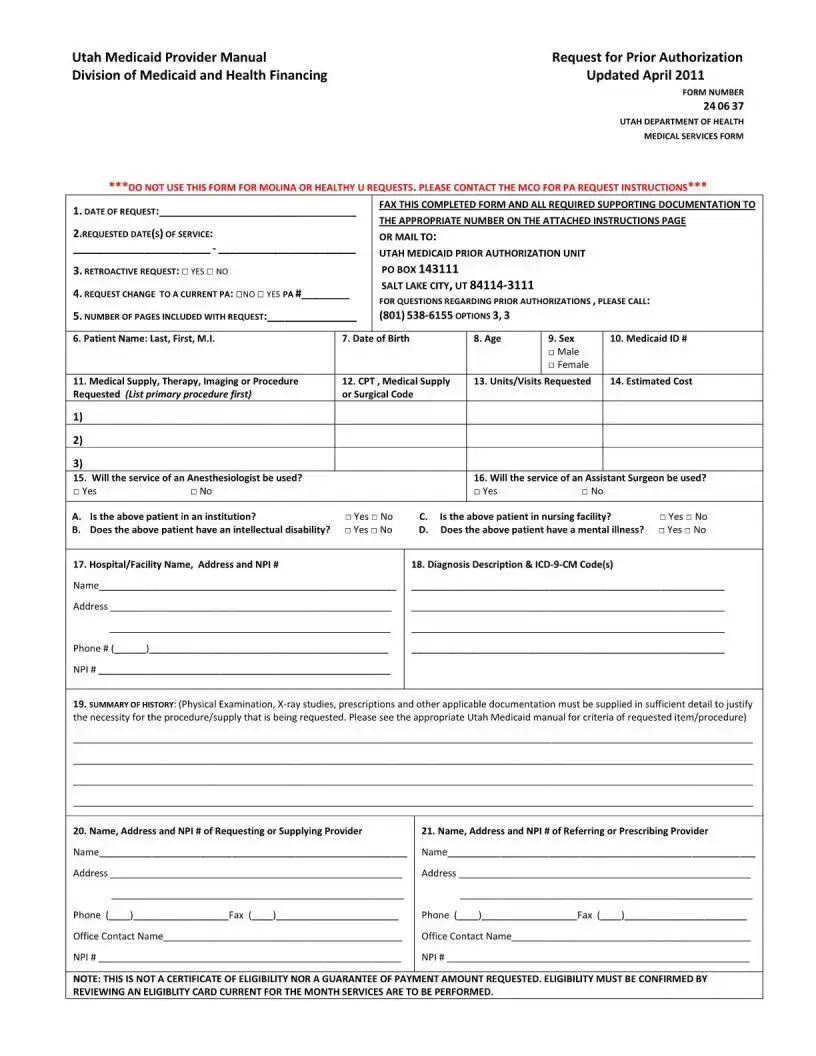
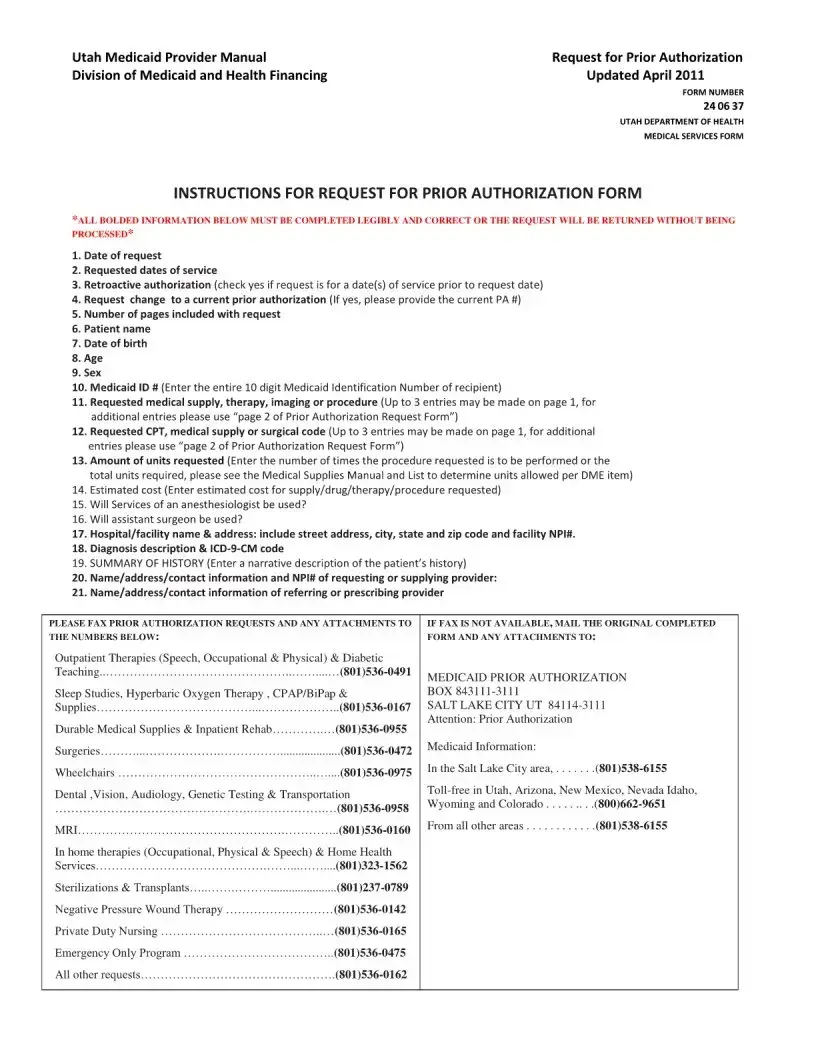
Filling out the Utah 24 06 37 form can be a daunting task, especially for those unfamiliar with the nuances of Medicaid prior authorization requests. One common mistake is neglecting to complete all required fields. Each section of the form is crucial, and missing even one detail can result in delays or denials. Ensure that all bolded information is filled out legibly and correctly to avoid having your request returned.
Another frequent error involves the Medicaid ID number. It's essential to enter the entire 10-digit number accurately. An incorrect ID number can lead to significant complications, including the rejection of the authorization request. Double-checking this information before submission can save time and frustration.
Many individuals also forget to specify the requested dates of service. This is critical because it helps determine the eligibility of the request. If these dates are missing or incorrect, it can lead to misunderstandings about the services being requested.
Additionally, some people do not provide a clear summary of the patient's history. This section is vital for justifying the necessity of the requested services. A detailed narrative that includes relevant medical history, examinations, and treatments can significantly strengthen the request.
Another common oversight is failing to indicate whether the request is for a retroactive authorization. If the request pertains to services provided before the submission date, this must be clearly marked. Otherwise, the request may be processed incorrectly.
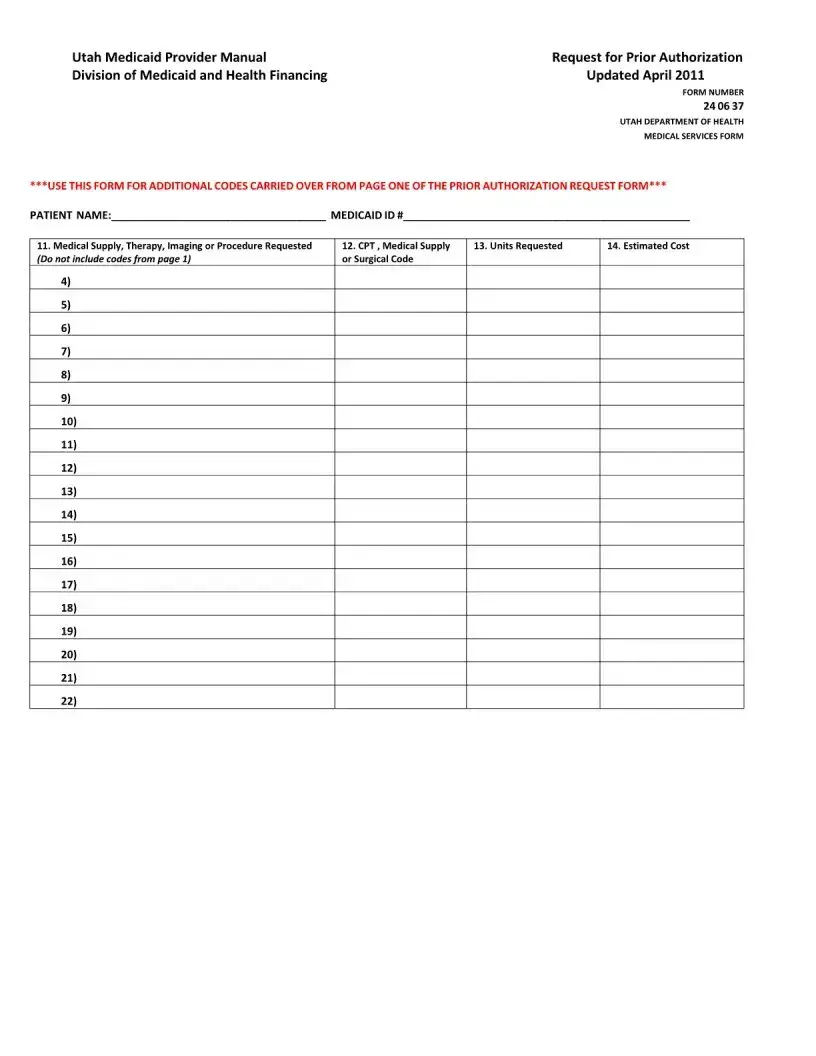
When listing the medical supplies or procedures requested, individuals sometimes do not prioritize their entries. The primary procedure should always be listed first, followed by any additional procedures. This helps streamline the review process and ensures that the most critical requests are addressed promptly.
Moreover, some individuals overlook the importance of including the estimated cost for the requested services. This information is necessary for the review process, and failing to provide it can lead to delays or denials of the request.
Another mistake involves not specifying whether services from an anesthesiologist or an assistant surgeon will be used. This information is vital for determining the scope of the procedure and ensuring all necessary resources are allocated.
Lastly, many applicants fail to include contact information for both the requesting and referring providers. This oversight can lead to confusion and delays in processing the request. Clear communication is key, so providing complete contact details is essential.
In summary, taking the time to carefully complete the Utah 24 06 37 form can make a significant difference in the authorization process. By avoiding these common mistakes, applicants can enhance their chances of a smooth and successful request.